
Research
For Acute Ischemic Stroke Patients, Clinical Trial at Marcus Neuroscience Institute Offers Hope for Improved Recoveries
3 min. read
An acute ischemic stroke is a medical emergency caused by decreased blood flow to the brain, which results in damage to brain cells. If that stroke victim does not receive medical treatment within a certain timeframe from the onset of symptoms, permanent neurological damage could occur, affecting speech, limb movement or cognitive abilities.
Avoiding such permanent disability with advances in minimally invasive procedures and medications is the goal of ongoing clinical trials and scientific research. The newest such trial is one undertaken by a few medical centers nationwide, including Marcus Neuroscience Institute at Boca Raton Regional Hospital, part of Baptist Health South Florida.
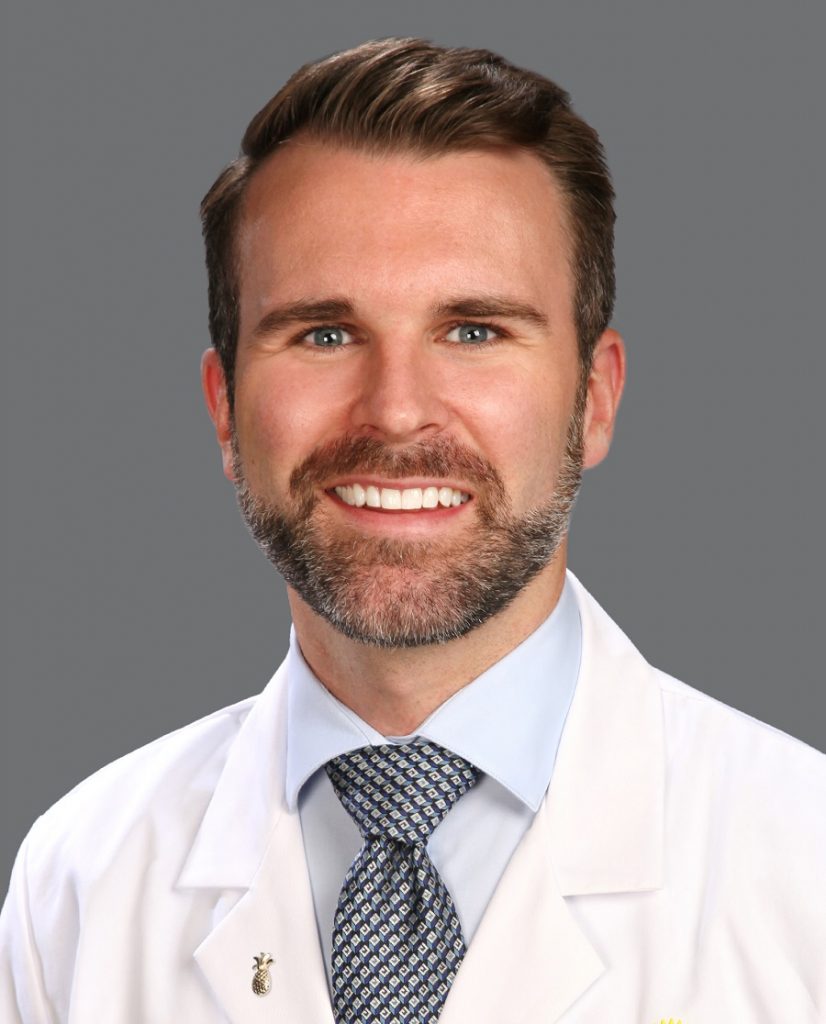
Brian Snelling, M.D., director of cerebrovascular and endovascular neurosurgery at Marcus Neuroscience Institute at Boca Raton Regional Hospital, a part of Baptist Health.
The goal of the trial is to evaluate the safety and tolerability of administering human bone-marrow-derived stem cells, known as NCS-01, to patients that have suffered so-called large vessel occlusions, which is when one of the major arteries of the brain is blocked. The NCS-01 treatment is administered after a mechanical thrombectomy, a minimally invasive procedure during which doctors remove blood clots using a device threaded through brain arteries.
The ideal patient candidate for the trial has undergone the thrombectomy within 48 hours of the onset of stroke symptoms, explains Brian Snelling, M.D., director of cerebrovascular and endovascular neurosurgery at Marcus Neuroscience Institute at Boca Raton Regional Hospital. Additionally, these patients who are candidates for the trial still have neurological issues, such as speech or movement problems -- even after the thrombectomy.
“We’re trying to look beyond what we can do from physically retrieving the clot,” said Dr. Snelling. “And find something else we can do to help these patients who have a brain that may be partially damaged or at risk, and help that brain go back to being normal -- versus that brain progressing to being dead tissue.”
The stroke patient, or the patient’s caregiver surrogate, will be offered participation in the trial. The trial is “randomized” — meaning there will be two primary groups of patients monitored: those who get the NCS-O1 treatment and those who get a placebo.
The human bone-marrow-derived stem cells, or NCS-01, have been shown in animal-based trials to be effective in reducing infarct volume and helping improve function in animals. Cerebral infarction volume is a measure of stroke severity, and related to neurological deficits. Determining infarcted brain tissue volume is an important element of clinical studies to establish the effects of potential therapies.
Once the stroke victim, or the patient’s surrogate, agrees to take part in the trial, Dr. Snelling and his team take immediate action.
“The patient then gets re-catheterized, and we put a tiny catheter up into the middle cerebral artery, the branch that had the stroke and had the clot that was pulled out during the thrombectomy,” explains Dr. Snelling. “Now, that artery is open and we inject the stem cells directly into the middle cerebral artery. Hopefully, these stem cells can prevent the brain from ‘completing the stroke.’ And, hopefully, the patient can get better.”
Farrah J. Wolf, M.D., a board-certified Interventional radiologist at Boca Raton Regional Hospital, is a member of the Institute’s stroke team performing endovascular interventions. With a strong background in clinical research, she is participating with Dr. Snelling in the NCS-01 trial. “Several weeks ago, I performed the first intra-arterial infusion procedure here at Boca Raton Regional Hospital on one of my ischemic stroke patients post-thrombectomy, and hope to continue to enroll patients over the upcoming months,” said Dr. Wolf.
Acute ischemic stroke is a leading cause of death and disability in the U.S., affecting about 700,000 people each year. Every 40 seconds, someone in the U.S. has a stroke, and every 3 minutes and 14 seconds someone dies of stroke, according to the U.S. Centers for Disease Control and Prevention (CDC). Ischemic strokes account for about 87 percent of all strokes, according to the American Stroke Association.
Dr. Snelling’s team will use the “NIH Stroke Scale” to measure the stroke victim’s neurological function and deficits. A score is determined after asking the patient certain questions and having him or her perform several physical and mental tests. This checklist of questions and tasks scores a person's level of alertness and ability to communicate and perform simple movements. Candidates for the NCS-O1 trial will have an NIH score of 6 or higher after standard-of-care treatment, such as the thrombectomy and any clot-busting medications that may be administered.
“We want to make sure the patient can tolerate the treatment – that’s the main objective,” said Dr. Snelling. “In addition -- from a bigger perspective -- this is just one small step out of a larger number of steps that will be undertaken to hopefully find something that can help these acute stroke patients from suffering long-term or permanent disabilities.”
Healthcare that Cares
Related Stories
View All Articles
Roundup: New ‘Risk Calculator’ Detects Heart, Stroke Risks; CDC on Declining Vaccinations Among Kindergartners; and More News
November 17, 2023
4 min. read

World Stroke Day: More Education Needed on Stroke Symptoms, Risk Factors and Prevention
October 26, 2023
4 min. read
Going Against the Flow: Innovative TCAR Procedure Lowers Stroke Risk
September 20, 2022
3 min. read