
Education
Cardiac Patient After Minimally Invasive Procedures: ‘How Do You Thank Someone for Saving Your life?’
5 min. read
Even with regularcare, heart disease can get very complicated and worsen suddenly. That was thecase with David Horovitz, who sought help at Miami Cardiac & VascularInstitute and discovered he had a near total blockage in the arterythat causes so-called widow-maker heart attacks.
After multiple interventionsthat included a balloon angioplasty and coronary stenting, followed later by a minimallyinvasive transcatheter procedure to replace his aortic valve, Mr. Horovitz, 77,is now feeling strong and is looking forward to the future.
“How do you thanksomeone for saving your life?” Mr. Horovitz asks. “Words cannot describe thecare I received. It was absolutely amazing.”

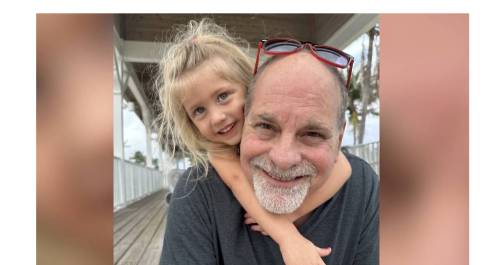
David Horovitz with his wife, Maria Luz.
Mr. Horovitz, who is diabetic, says he was already under a cardiologist’s care for conditions that included an arrhythmia and problems with his mitral valve, which was allowing blood to flow in the wrong direction in his heart. He thought he had those conditions under control, but he noticed he was feeling weaker and weaker.
“It was so badthat I couldn’t walk more than 20 feet without getting out of breath or havingto sit down,” he recalls. “I couldn’t even take out the garbage. I couldn’t doanything.”
While he wasconcerned, he didn’t realize yet how serious it was.
Diagnosing the problems
Mr. Horovitz sought help frominterventional cardiologist Phillip Erwin, M.D.,PhD., whofounded the Institute’s transcatheter aortic valve replacement (TAVR) programat South Miami Hospital.
Tests revealed a problem with the aortic valve and a severe blockage in Mr. Horovitz’s left anterior descending (LAD) artery, which supplies blood to the larger, front part of the heart. Because it serves such a big portion of the heart, the LAD artery is a particularly dangerous place to experience a blockage — which is why heart attacks that originate there have been nicknamed “widow-makers.” Although not always fatal, such heart attacks can cause lot of damage to the heart muscle if blood flow isn’t restored quickly.
“When they told me it was 98 or 99 percentoccluded, I understood immediately why I couldn’t walk and I couldn’t breathe,”said Mr. Horovitz, a former respiratory therapist who manages a large pulmonarymedical practice. He is familiar with the heart’s anatomy — and the danger hefaced. “It’s the main aorta of the heart. If it’s occluded, or blocked, youwould be in imminent danger of having a heart attack and could pass away.”
A multi-prongedapproach
Helping Mr. Horowitz required a two-staged, minimally invasive approach that used his blood vessels as a super highway to reach his problem area without having to undergo the trauma of open-heart surgery. “He was not a surgical candidate because his heart was so weak,” explains Dr. Erwin, the director of complex coronary and structural interventions at South Miami Hospital.
In the firstprocedure, Dr. Erwin used a catheter to temporarily insert the world’s tiniestheart pump, called an Impella,into Mr. Horovitz’sleft ventricle to keep blood moving while he worked. “It’s sort of likea backup generator for the heart,” he explains. “It does some of the work forthe heart, so that while you are fixing blocked vessels and reducing theheart’s blood flow, the body still has some support.”
Dr. Erwin then threadeda miniature diamond-tippeddrill called a Rotoblader toward Mr. Horovitz’s heart, startingat a vessel in his groin. The drill was used to break up the hardened blockagein a procedure called a rotational atherectomy. “The plaque blockinghis artery was so highly calcified, it was like cement in there,” Dr. Erwinexplains. Once the drill broke up the blockage, Dr. Erwin did an angioplasty,expanding a balloon in the artery to restore blood flow and then placing a stentto support the wider opening. Mr. Horowitz went home the next day.
About a monthlater, after his heart grew a bit stronger, Mr. Horowitz returned to SouthMiami Hospital for a transcatheteraortic valve replacement (TAVR) with Dr. Erwin.
During thisminimally invasive procedure, a new folded-up valve is inserted through acatheter and deployed in place of the old, diseased valve without having to cutopen the chest. Miami Cardiac & Vascular Institute specialists participatedin clinical trials for this technique and were instrumental in developing thistechnology. Originally designed as an intervention of last resort for thesickest and most fragile patients, the procedure was approved by the FDA lastyear for wider use among even low-risk patients because of the potentialadvantage of avoiding open-heart surgery. TAVR is offered is BaptistHospital, BethesdaHospital East, and Boca Raton RegionalHospital, as well as South Miami Hospital.
A gratefulfamily
Mr. Horovitz, whowent home the next day, says he was feeling better before he even left thehospital. “I couldn’t believe it. I got out of bed and with the help of my wifeand the nurse, and I was able to walk again,” he says. And he has continued hisjourney toward better health. “I’m not going to say I run around the block, butI can walk around the block five times now without getting out of breath.”
Mr. Horowitz is gratefulto the Institute and South Miami Hospital for the care he received, but he is especiallyappreciative of Dr. Erwin, who he described as very compassionate as well asskilled. Upon noticing Mr. Horovitz’s worried wife, Maria Luz, was crying asher husband was prepped for the TAVR procedure, Dr. Erwin pulled her aside fora reassuring hug. He promised to care for Mr. Horowitz as if he were his ownfather. “You have noidea how much that meant to my wife,” Mr. Horowitz says. “That’s the kind ofperson Dr. Erwin is.”
The right place for treatment
It is for complicated casessuch as Mr. Horovitz’s that the Complex Percutaneous Coronary Interventionprogram was established at Miami Cardiac & VascularInstitute.“The physicians have a long history of implementing cutting edge technology andinnovative procedures,” says interventional cardiologist Ramon Quesada, M.D., medical director ofStructural Heart and Complex Percutaneous Coronary Intervention at theInstitute. A pioneer of hybrid procedures for complex cardiac cases, Dr.Quesada has been at the forefront of the design,development and implementation of new techniques.
Thanks to the Institute’sinvolvement in clinical research, patients have access to new technology yearsbefore they would at other regional hospitals, he says. “Our involvement inclinical research over the years in both interventional and structuralcardiology, as well as minimally invasive heart surgery, has laid the groundworkfor better care.”
Healthcare that Cares
Related Stories
View All Articles
Structural Heart Disease: The Rapid Pace of Advances in Replacing, Treating Heart Valves
February 12, 2024
5 min. read
Second Heart Valve Replacement Returns Patient to Active Life
February 7, 2024
3 min. read

How to Avoid 'Holiday Heart Syndrome' and Other Cardiac Events This Time of Year
December 19, 2023
4 min. read